The first case in the province was leading in the country! Supported by the "Flying Dragon DSA" cath lab, the "one-stop" hybrid surgery for severe coronary heart disease was here
Hits: 3149 Time: 2019-08-13
On July 30, the first patient in Zhejiang Province underwent a “one-stop” hybrid surgery for severe coronary heart disease under the support of the “Flying Dragon DSA” catheterization laboratory was discharged from the hospital. "Thank you to the doctors and nurses here. You have thought about the patients and found the best surgical plan for me. Treating patients like relatives. I really appreciate you from the bottom of my heart." Ms. Tang (pseudonym) said emotionally.
Since the discovery of severe coronary heart disease in March, Ms. Tang and her family have been worried for fear that a fatal accident might happen any day. Coronary angiography showed 99% stenosis in the middle of the left anterior descending branch of her heart, diffuse stenosis in the proximal right coronary artery, 90% stenosis at the most severe part, 95% stenosis at the distal end, and 100% occlusion at the far end. Before she was a difficult multiple-choice question: Take medicine? Intracardiac interventional surgery? Extracardiac bypass surgery?
The doctors are kind. From the perspective of the patient, our doctor should not only help her cure the disease, but at the same time help her relieve her pain, and maximize the advantages of drugs, interventional therapy and surgical treatment. By the director of the heart center of our hospital, the director of cardiovascular internal medicine, the chief physician, Tang Lijiang, the deputy director of the cardio-macrovascular surgery of our hospital (presiding the work), the chief physician He Renliang, the chief expert of cardiac surgery in our hospital, the Shanghai Renji Hospital, and the professor Xue Song , formed the heart center team, which brought together multidisciplinary experts from our hospital to discuss this patient specifically. Finally, they decided to perform thoracoscopic-assisted small-incision anterior descending coronary artery bypass + percutaneous interventional treatment of the right coronary artery hybrid operation for Ms. Tang. This operation fully realized the advantages of small trauma and long use time of interventional and small-incision internal mammary artery surgical bypass, and maximized the patient's benefit after treatment.

Composite technology, one-stop shop, and small incisions constituted multiple first in our hospital
The so-called hybrid surgery, also known as compound technology, is a cutting-edge technology in the heart field that has emerged in recent years. It is the combination of intracardiac intervention and surgery performed on the same patient, combining the original “divide-and-conquer” surgery for heart disease, cardiology interventional therapy and imaging diagnosis, etc., and implement them at the same time, so as to achieve a healing effect of 1+1>2.
The reason why Ms. Tang cold undergoes hybrid surgery in the hybrid operating room in Sandun Hospital was because it had the first Siemens ARTIS pheno "Flying Dragon" DSA (angiography machine) in Zhejiang Province and the third installed in the country, which integrated surgical operations , interventional therapy and imaging diagnosis, with clear images and high resolution. It provided real three-dimensional images for observing vascular disease, vascular stenosis, positioning measurement, diagnosis and interventional therapy, and provided necessary conditions for various interventional therapy.
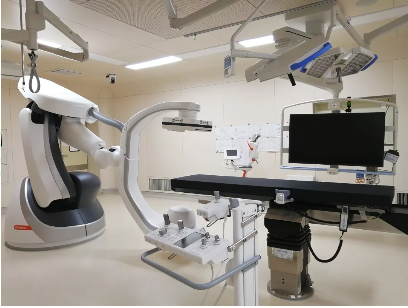
According to Dr. Wang Hongmei, deputy director of the Department of Anesthesia and Surgery of our hospital, the hybrid operating room in the Sandun hospital area is about 100 square meters, but there are 20-30 million worth of equipment. Except for DSA, the hybrid operating room also has a large number of equipment such as laparoscopes, high-pressure syringes, electrosurgical units, anesthesia machines, monitors, extracorporeal circulation machines, defibrillators, autologous blood recovery machines, monitors, etc., running at the same time, with more than 12 signal sources. The use of advanced signal digital processing system is convenient for doctors to access patient information at any time, to provide adequate hardware support for hybrid surgery.
On July 14th, a cardio-macrovascular surgeon in the heart center team of our hospital took the lead to perform the internal mammary artery-anterior descending artery bypass graft after a 10cm incision was made in the fourth intercostal space on the left side of the patient. This is to relieve the patient from the danger of the left anterior descending branch, the most important one of the three main blood vessels of the heart, restore blood flow and provide a safety guarantee for subsequent interventional treatments. Subsequently, an interventional expert in cardiovascular medicine performed coronary angiography for Ms. Tang to ensure that the internal mammary artery-the anterior descending artery was unobstructed, a cardiac stent was implanted in her right coronary artery to restore the normal blood supply to the heart.
The entire hybrid operation ended successfully after about two and a half hour, and Ms. Tang's heart "time bomb" was successfully lifted. The success of this operation is an affirmation of our hospital's heart center team, anesthesia surgery department, critical care medicine, radiology and other multi-department teams to participate in, cooperate, and solve complex and difficult cases. At the same time, it has also created many “the first time” of multiple departments in multiple hospitals. The hybrid operating room of the anesthesia surgery department ushered the true hybrid surgery patient for the first time. An expert in cardiovascular medicine implanted a stent under the guidance of the first Siemens ARTIS pheno "Flying Dragon" DSA in the province for the first time. And an expert in cardio-macrovascular surgery achieved vascular bypass with the aid of endoscopy to complete the operation with a small incision for the first time.

Science time
01 What is coronary artery hybrid surgery
Coronary hybridization surgery is undoubtedly the gospel for those patients who suffer from complicated and high-risk coronary artery disease. The emergence of this kind of cardiac hybrid surgery breaks the barriers between disciplines, combines the advantages of the heart and the heart, and enables more effective treatment of multivessel coronary artery disease, congenital heart disease and various complicated heart diseases, and reduces surgical trauma and mortality, and the incidence of postoperative hemiplegia.
02 How to make a small incision
Traditional heart bypass surgery starts with an incision in the chest, and the heart is exposed after the sternum is incised. Under normal circumstances, the incision in the chest of patients with traditional heart bypass surgery is about 20 cm long, and the sternum must be split. However, the small incision surgery of internal mammary artery-anterior descending branch bypass surgery requires only a 10cm incision among the ribs, without splitting the sternum. This greatly reduces the trauma to the patient, undoubtedly thanks to the assistance of thoracoscopic surgery technology. The technique of thoracoscopic surgery (video assisted thoracoscopic surgery) is regarded as one of the major breakthroughs in thoracic surgery in the last century. Its direct advantages include small surgical wounds, light postoperative pain, low impact on lung function, and small impact on immune function, which is more conducive to postoperative recovery.
03 Benefits of one-stop surgery
Coronary hybrid surgery can be one-stop (surgery hybridization and interventional surgery performed simultaneously in the same hybrid operating room at the same time) and split surgery (surgical bypass and interventional treatment at different time points). This gives full play to the advantages of long service life of the arterial bridge, small incision, and minimally invasive interventional therapy. One-stop surgery is usually performed by small surgical incisions first, followed by interventional stent treatment, which can verify whether the arterial bridge is unobstructed by angiography and reduce the risk of bleeding during surgery. Since interventional treatment, imaging examination, and surgical treatment are all performed in the same operating room, the waiting period for empty windows between operations is saved, and the economic burden of patients can be reduced. One-stop combined coronary heart disease surgery combined with internal surgery under the assistance of endoscopy has extremely high requirements for hospital equipment and doctors' technology. Only a few hospitals and doctors in China can carry out this, which is a leading level in China.
The patient was transferred to the general ward on the second day after surgery
The patient can go to the ground for activities on the 3rd day
If Ms. Tang’s condition is resolved by dividing and conquering heart disease according to the previous method of “divide and conquer”, her condition is likely to change while waiting for the second operation. However, as a beneficiary of the coronary artery hybrid surgery supported by the "Flying Dragon" DSA in our hospital, she does not need to be transferred between operating rooms and does not require multiple anesthesia, which greatly reduces the risk of surgery and postoperative complications. In the case of ensuring the effect of the operation, the risk of the operation is reduced, and the postoperative incision is also small, which is more conducive to her recovery. In addition, it also greatly saves the treatment cost.
She was transferred to the Intensive Care Unit (ICU) after the operation. Although her condition was stable, the chief physician Cai Guolong, the director of the ICU (2) of our hospital, who cared about the patient, gave up rest and guarded all night. That night, Ms. Tang successfully unplugged the tracheal intubation. For this patient, the ICU team focused on three areas: The first is the hemodynamics of the patient after cardiac surgery, the protection of the transplanted blood vessels and the stable perfusion of the heart, etc. The second is the patient's bleeding. Because during the operation, the patient has bleeding and used a lot of anticoagulant and antiplatelet drugs, the observation of postoperative bleeding is the top priority. To keep all kinds of drainage tubes unobstructed, monitor the amount and color of bleeding every hour. The third is to transfer the patients to the ward after endotracheal intubation, and give them adequate analgesia and sedation to alleviate postoperative anxiety and discomfort. At the same time, in order to prevent complications such as ventilator-related pneumonia, the ICU team conducted offline training on the patient under the premise of ensuring the patient's oxygen supply, and finally successfully offline, the patient was transferred to the general ward the next day. Chief physician Xu Qianghong, the deputy director of the ICU (2) of our hospital, introduced.

I saw Ms. Tang in the ward on the 8th day after the operation. She said that she could walk, eat and sleep. "Thank the doctors for removing the heart'time bomb' for me." In addition, she also specially praised the ward environment of Sandun Hospital, which was clean, refreshing and quiet, which gave her a good rest. Dr. Chen Shaoxi from the Department of Cardiovascular Surgery in our hospital said that Ms. Tang was able to go to the ground on the third day after surgery. After the wound was removed, she was discharged from the hospital and returned home.
Source: Department of Cardiovascular Medicine, Cardiovascular Surgery, Department of Critical Care Medicine, Department of Anesthesiology
Written by: Wu Linglong, Propaganda Department of United Front Work Department